AMDS™
HYBRID PROSTHESIS
Elevate the Standard.
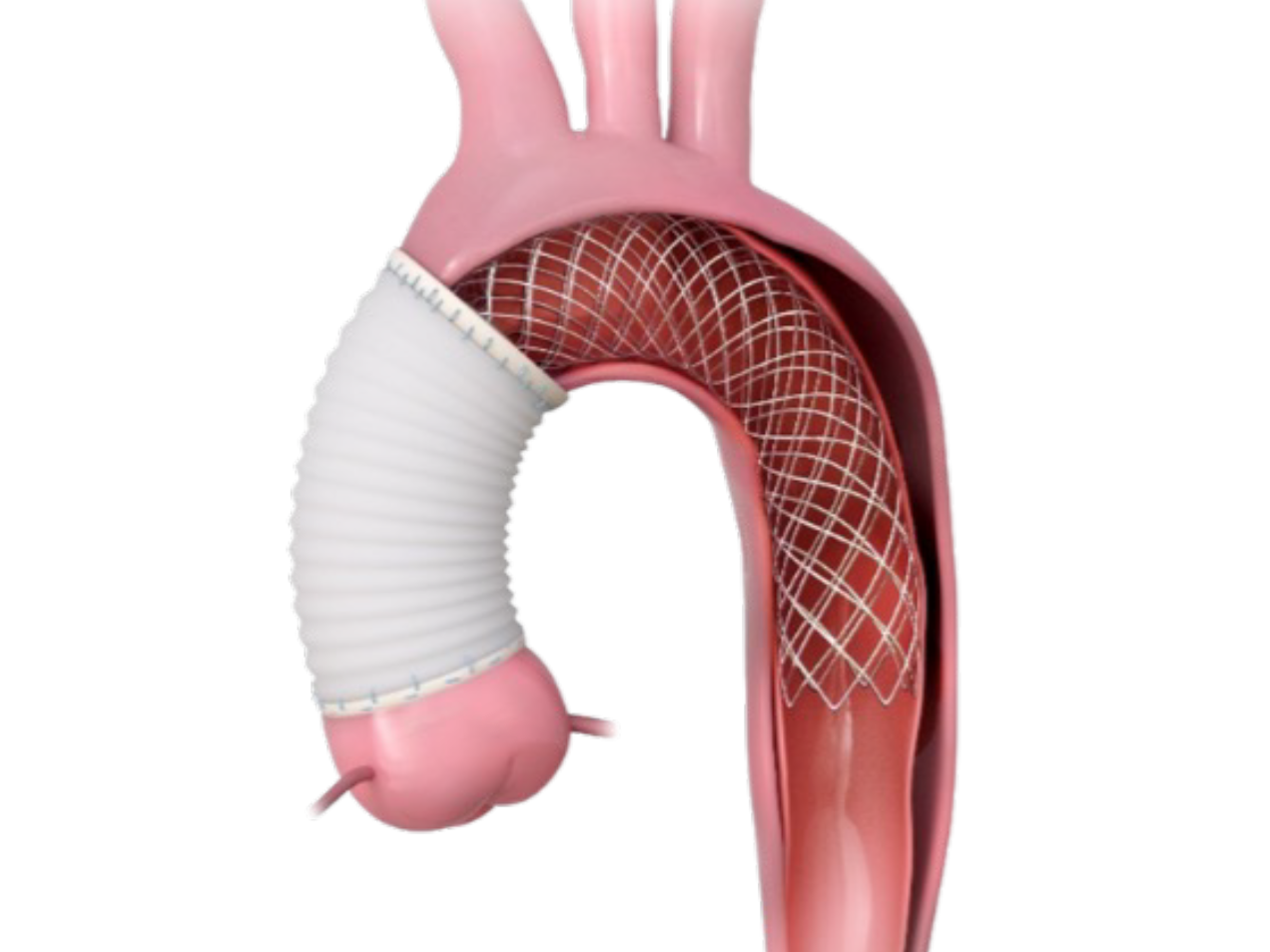
The world’s first device designed specifically to address the unique challenges of acute type A aortic dissection, specifically DeBakey Type I (ATAD I).
Product Highlights
-
DANE Prevention – The stent-supported cuff of the AMDS and expansion of the device from the arch distally elevates and support the intimal flap. This reduces tension on the intima, media, and the suture line, avoiding the formation of DANEs in the friable anastomosis.1, 2
-
Positive Aortic Remodeling – By avoiding DANE and stabilizing the true lumen, AMDS induces positive aortic remodeling, defined by 3 key measures: true lumen expansion, false lumen reduction, and total aortic diameter stabilization.3
-
Malperfusion Resolution – AMDS-induced expansion of the true lumen demonstrates effective resolution of vessel malperfusion.1
-
Uninhibited Flow to Supra-Aortic Vessels (SAVs) – The novel stent design of AMDS allows for uninterrupted flow into the native SAVs without surgical manipulation (i.e., bypass).1
-
Minimal Time Added to Operation – AMDS prolongs the circulatory arrest time of the hemiarch procedure by only a few minutes, with additional time for suturing, without adding significant technical complexity.1,4
Product Overview
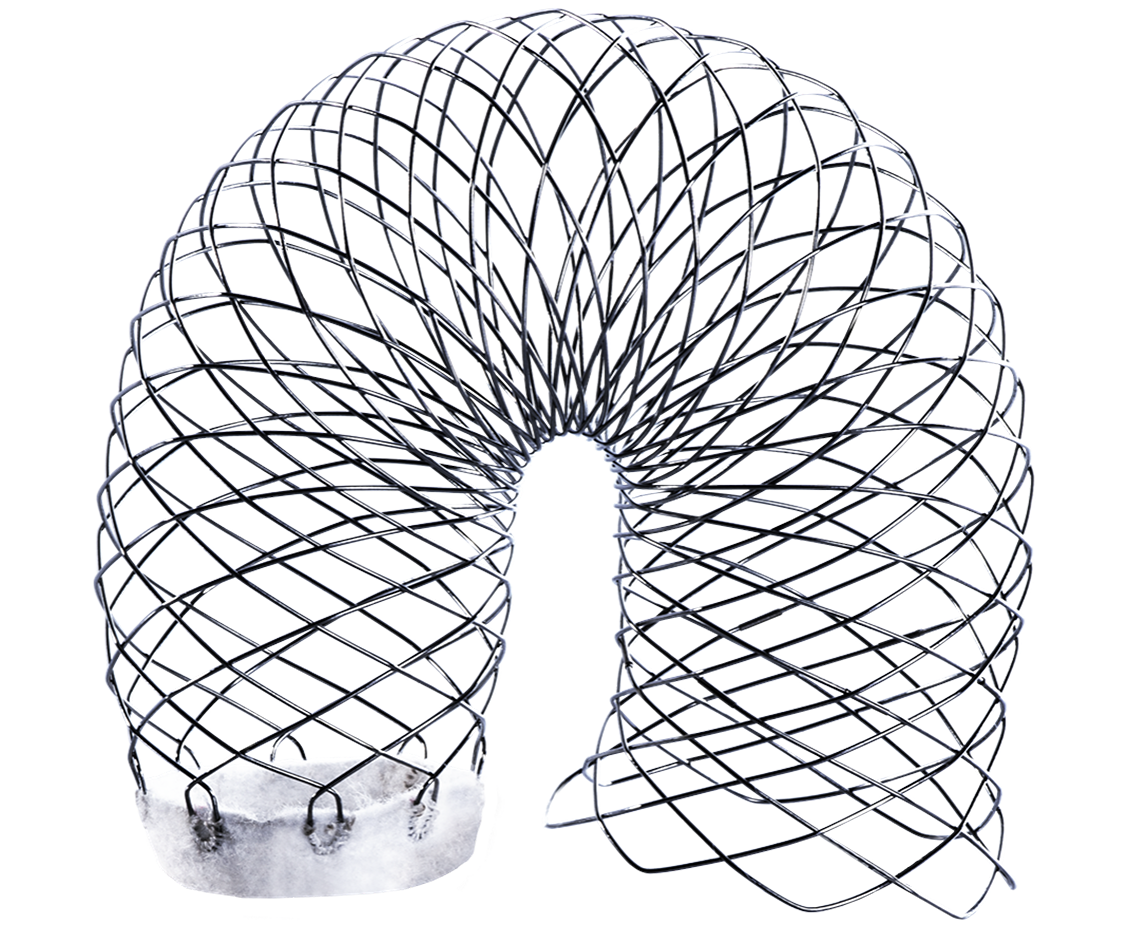
1. PTFE FELT CUFF

Component made of a PTFE felt tube is used to buttress and strengthen the aortic tissue in preparation to perform the conventional polyester graft to aorta anastomosis.
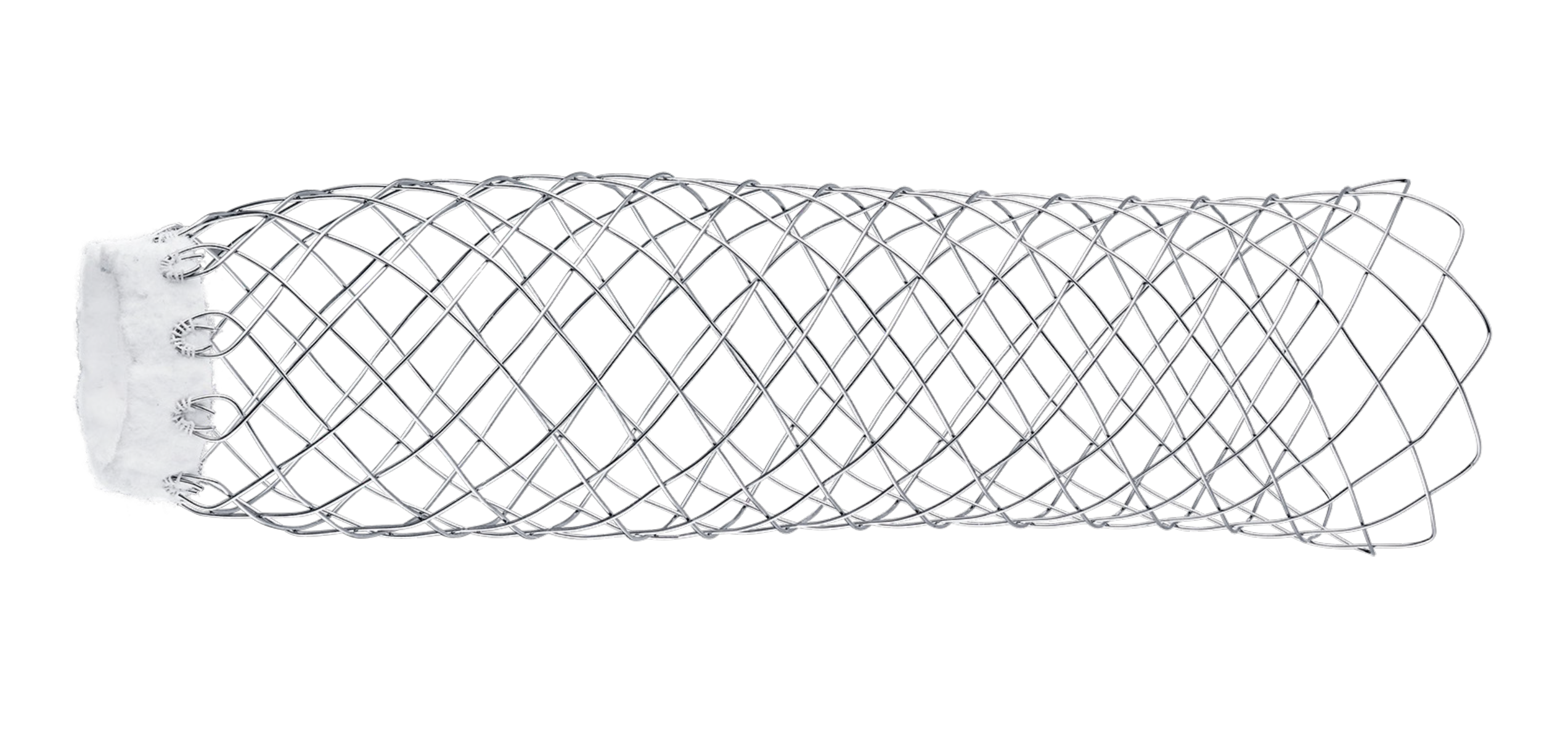
2. UNCOVERED NITINOL WIRE BRAIDED STENT
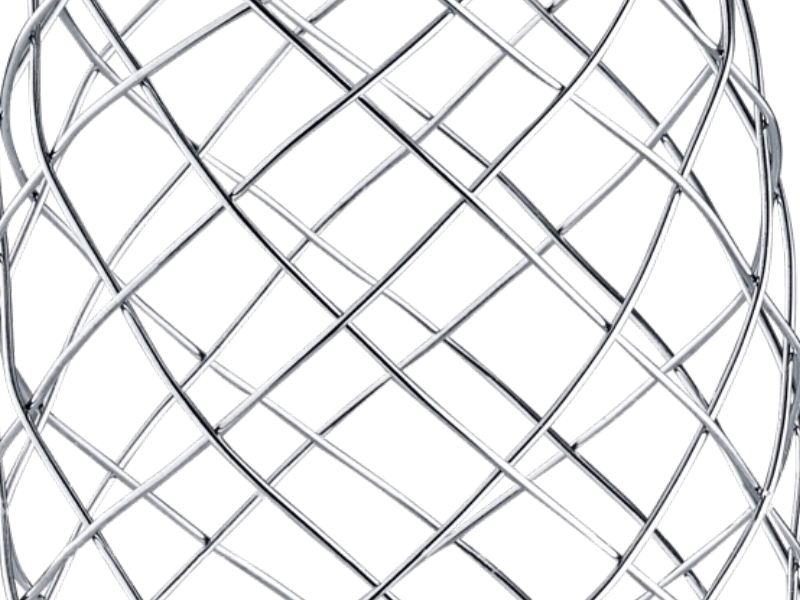
Expands and supports the true lumen across the aortic arch and descending aorta thereby stabilizing the aortic wall and promoting remodeling.
3. STENT SUPPORTED CUFF

The stent supported cuff of the AMDS and expansion of the AMDS from the arch distally, elevates and supports the intimal flap, reducing the tension on the suture line, avoiding the formation of DANEs in the friable anastomosis.
4. DESIGNED TO AVOID dSINE
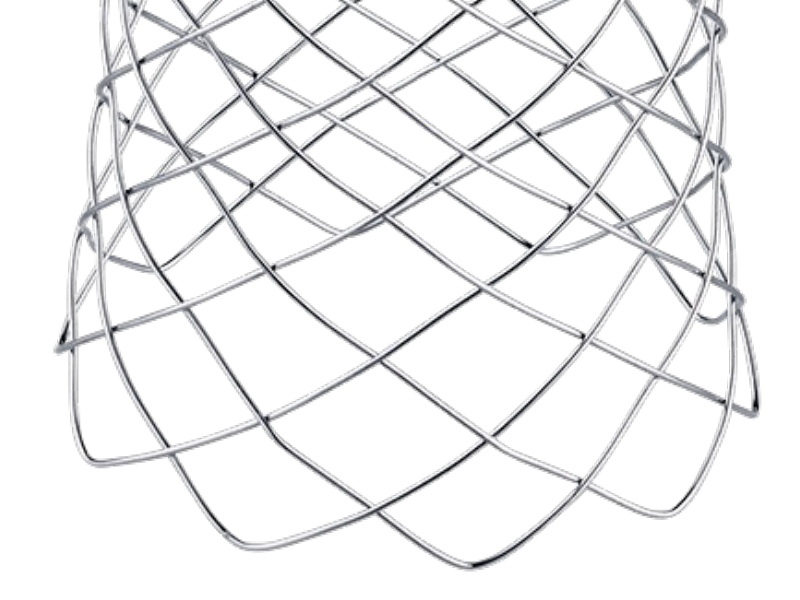
When deployed in vessel, the distal ends of the stent are designed to point away from the aortic wall to avoid dSINEs.
1. RED CAP
Not functional.
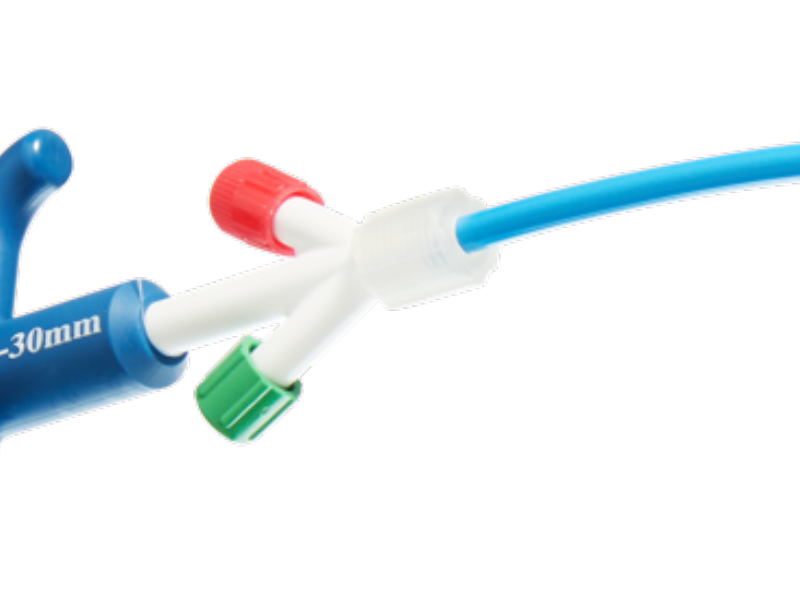
2. GUIDEWIRE (GW) EXIT
Compatible with 0.035” GW (optional).

3. HANDLE
Ergonomic handle for easy grip during delivery.

4. GREEN CAP
To deploy/release the suture constraining the stent.
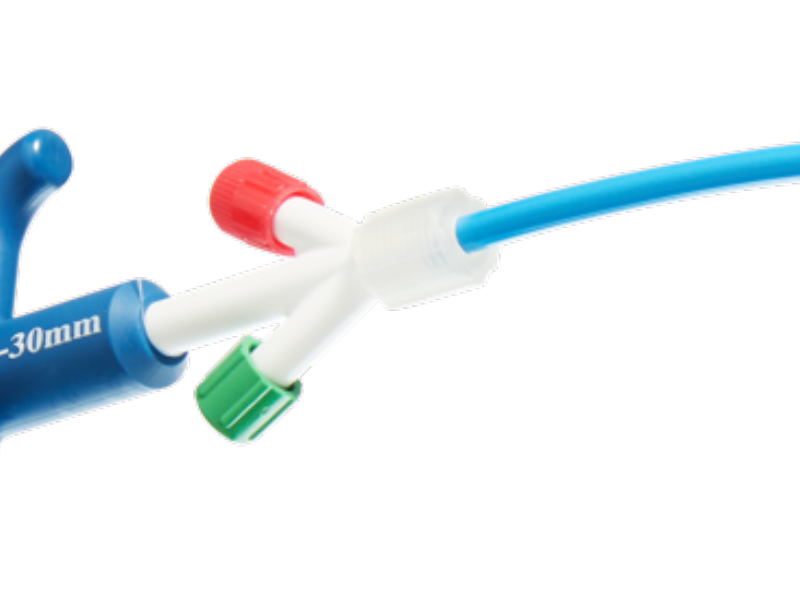
5. PROTECTIVE SHEATH
For simple and atraumatic introduction to the transected aorta (6 cm long).

6. LOADED STENT
Flexible catheter shaft for simple tracking of system and atraumatic to vessel.

7. PIGTAIL SHAPED TIP
Pigtail tip reduces risk of device tracking into FL via a entry tear/fenestration.


“Knowing that you’re giving people surgery that is not having any additional complexity but with a better outcome is very reassuring.”
A new tool in the toolbox for surgeons to do a better operation at the time of an index operation for a DeBakey I.
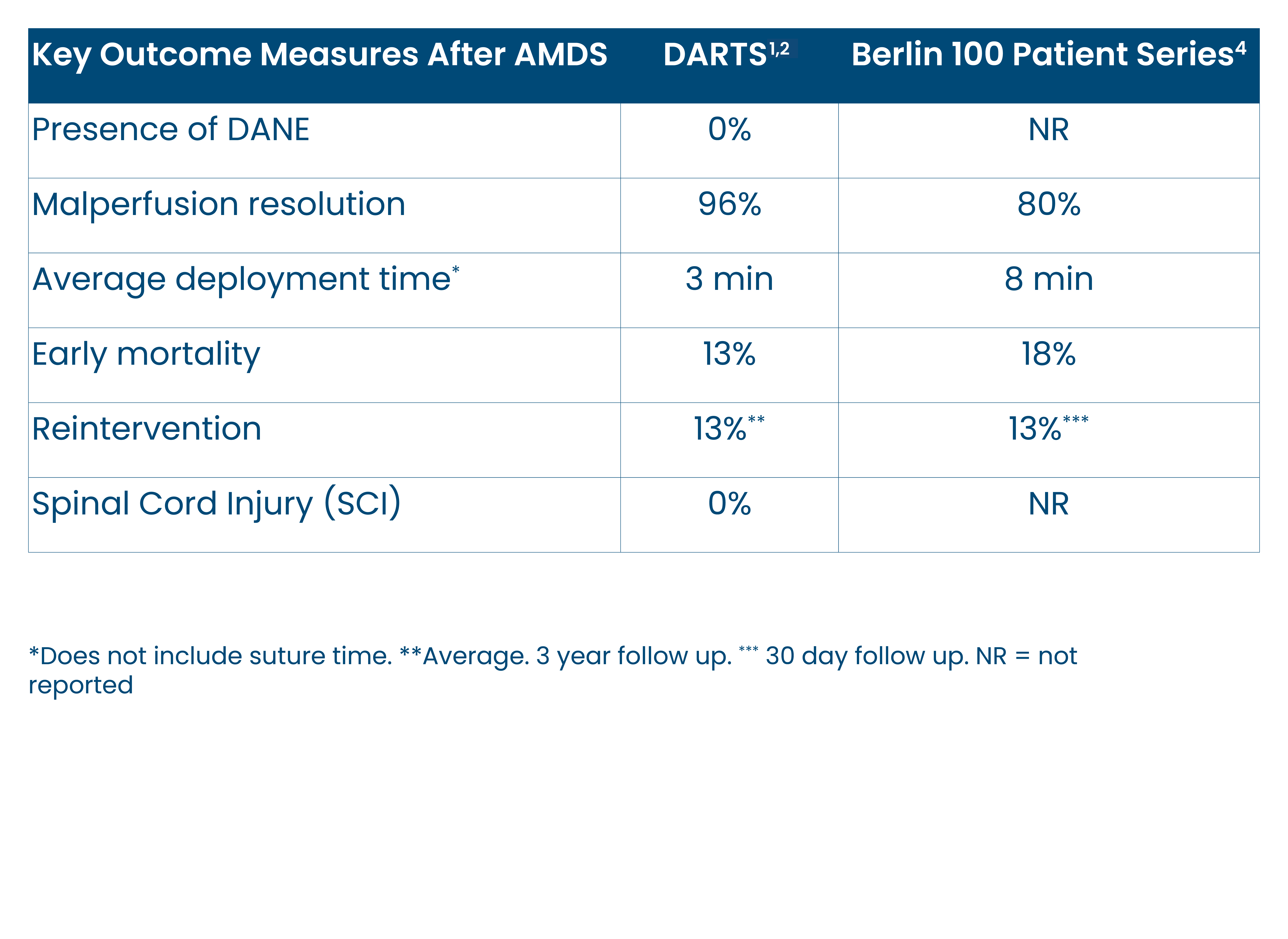
Clinical Evidence
Proven Clinical Results
- AMDS Prevents DANE and Resolves Malperfusion, Inducing Positive Aortic Remodeling.
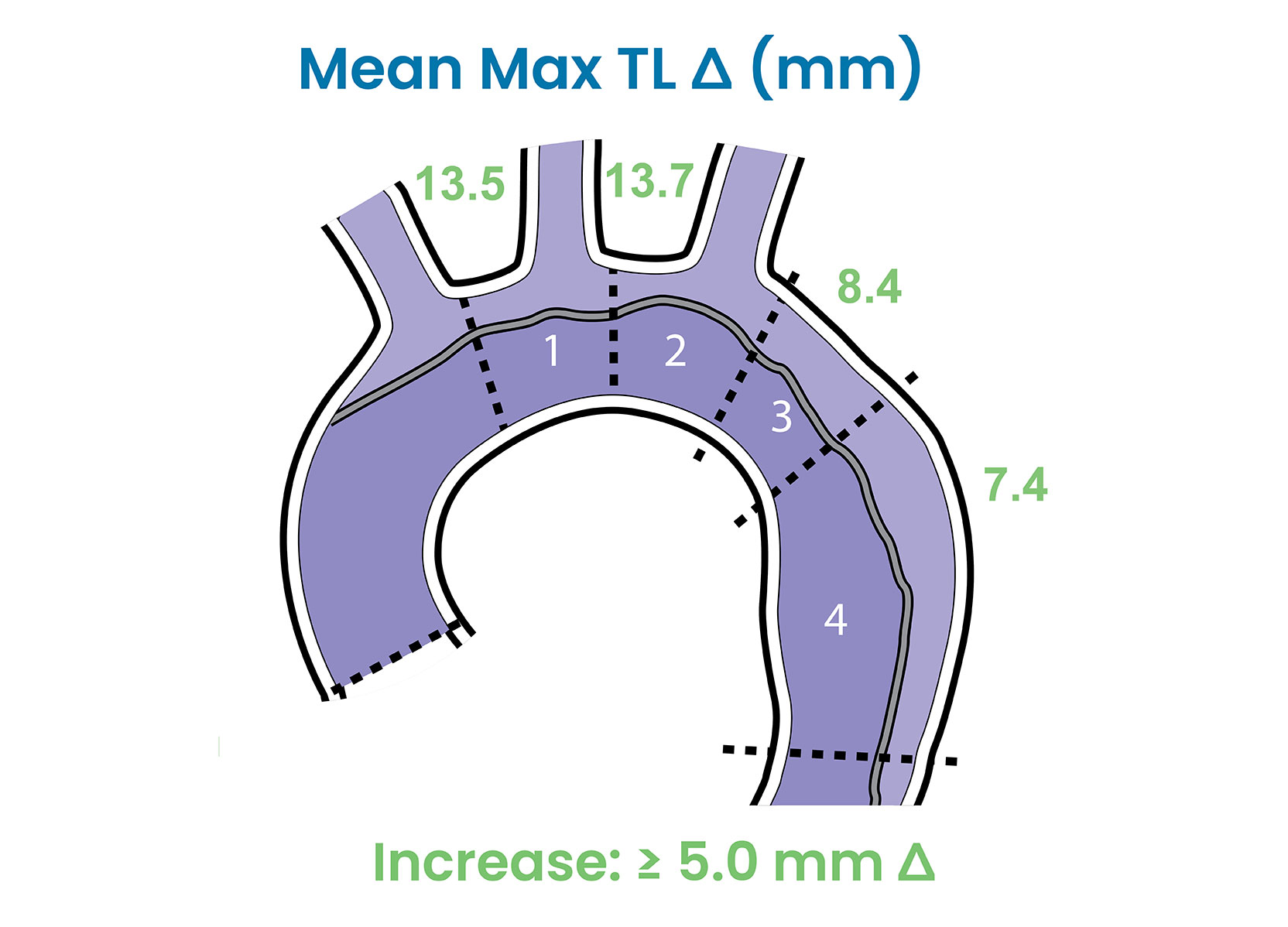
True Lumen Expansion
- DARTS study demonstrated sustained true lumen expansion ≥ 5.0 mm in aortic Zones 1-4 from pre-op to 3 years, post-op. 3
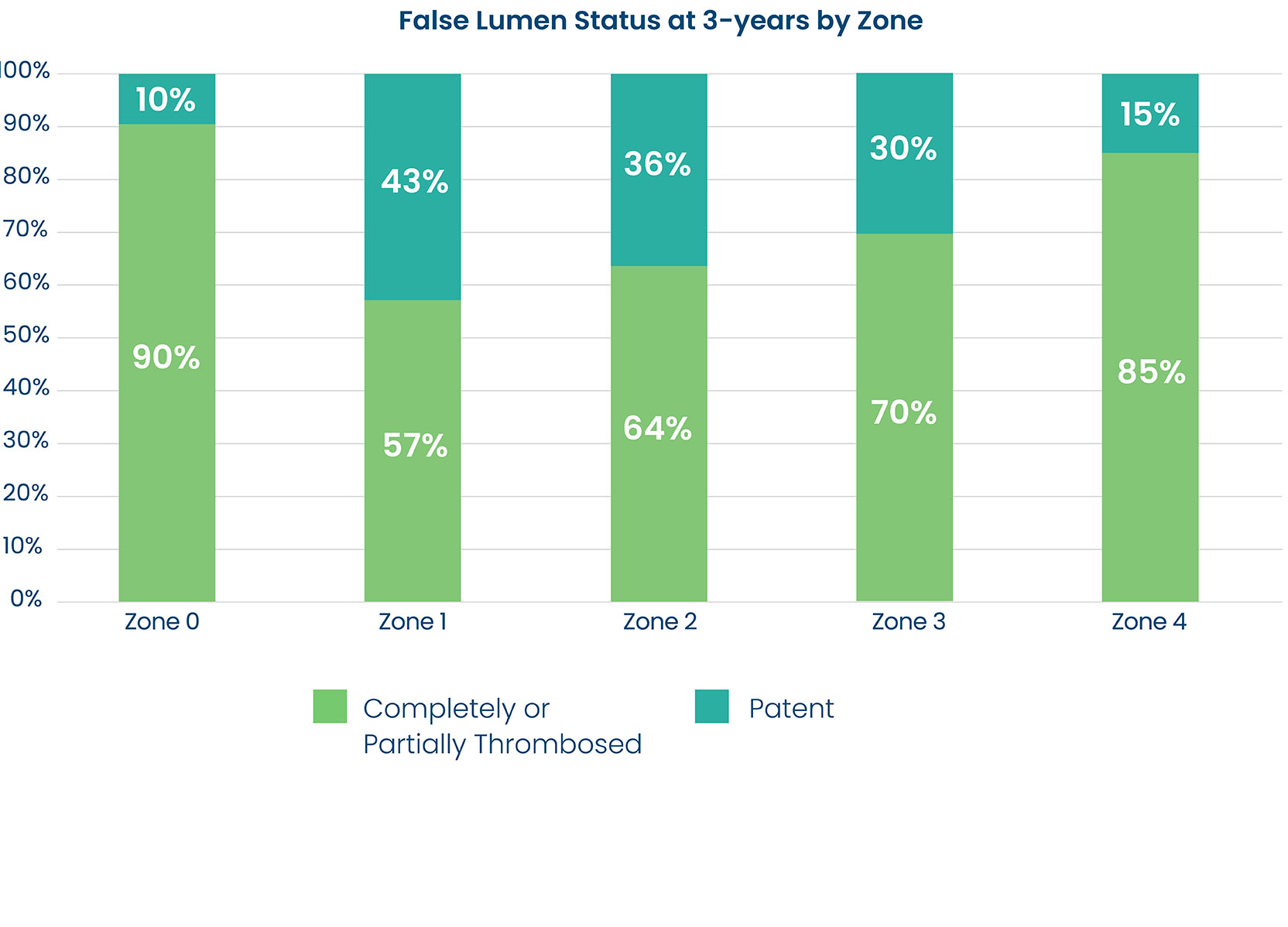
False Lumen Reduction
- DARTS study demonstrated complete or partial false lumen thrombosis in the majority of patients in Zones 0-4 at 3 years post-op.3
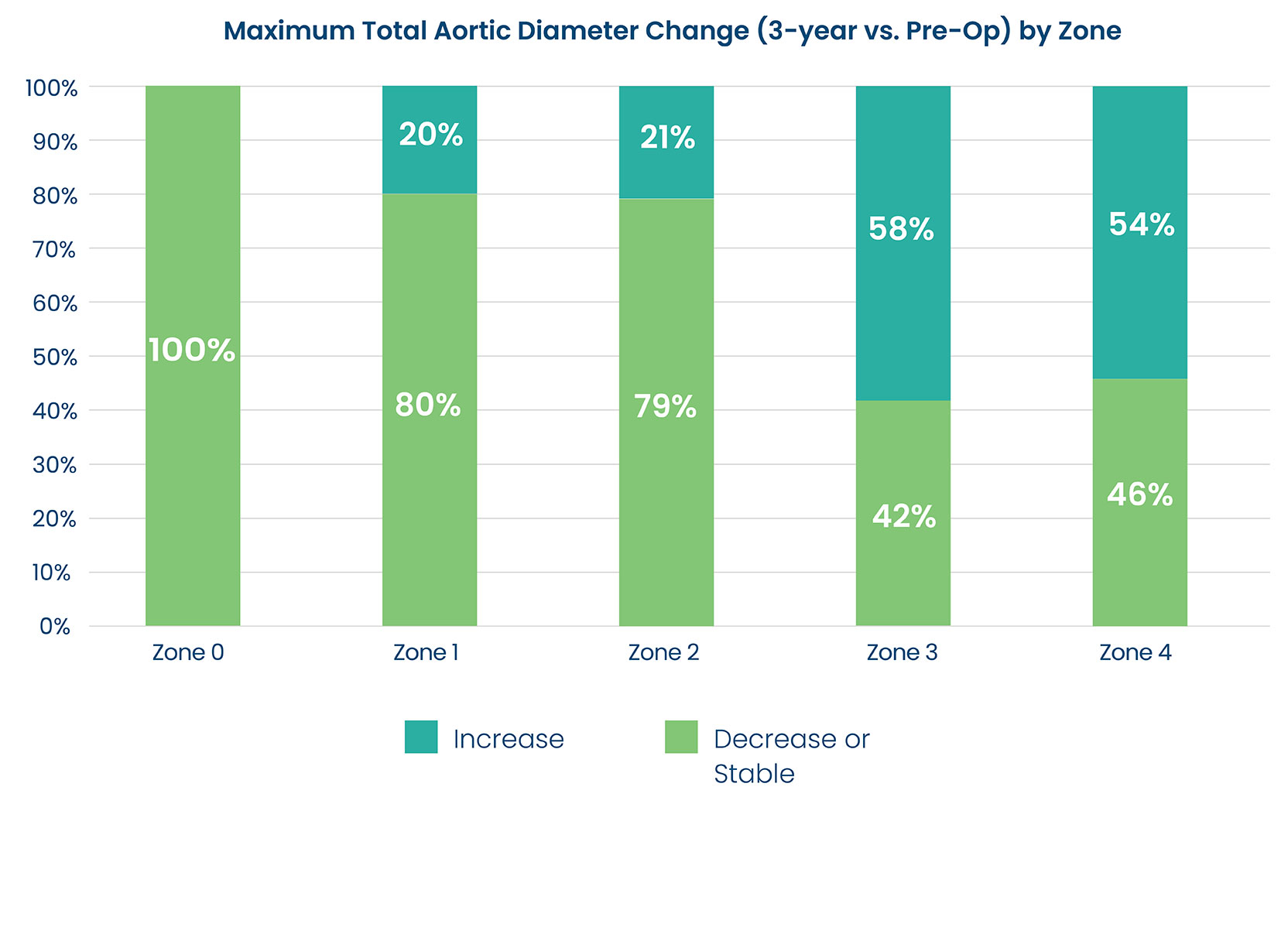
Total Aortic Diameter Stabilization
-
DARTS study demonstrated total aortic diameter stability or decrease in a majority of patients in Zones 0-2 and half of the patients in Zones 3 and 4 at 3 years, post-op.3
Additional Resources
Explore additional resources for AMDS below. For further information or to contact a sales associate in your area, contact us.
- Bozso, Sabin J., et al. “Three-year outcomes of the dissected aorta repair through stent implantation trial.” The Journal of Thoracic and Cardiovascular Surgery (2022).
- Bozso, Sabin J., et al. “Midterm outcomes of the dissected aorta repair through stent implantation trial.” The Annals of Thoracic Surgery 111.2 (2021): 463-470.
- DARTS Internal Data On File.
- Montagner, Matteo, et al. “The arch remodelling stent for DeBakey I acute aortic dissection: experience with 100 implantations.” European Journal of Cardio-Thoracic Surgery 62.2 (2022): ezac384.
CAUTION: Investigational Device. Limited by Federal (or United States) law to investigational use. All products and indications are not available/approved in all markets. All trademarks are owned by Artivion, Inc. or its subsidiaries. On-X Life Technologies, Inc., Jotec GmbH, and Ascyrus Medical GmbH are wholly owned subsidiaries of Artivion, Inc. MLENG1586.000. (2023-04)
| Ascyrus Medical GmbH, Bethmannstrasse 8, 60311 Frankfurt, Germany |

